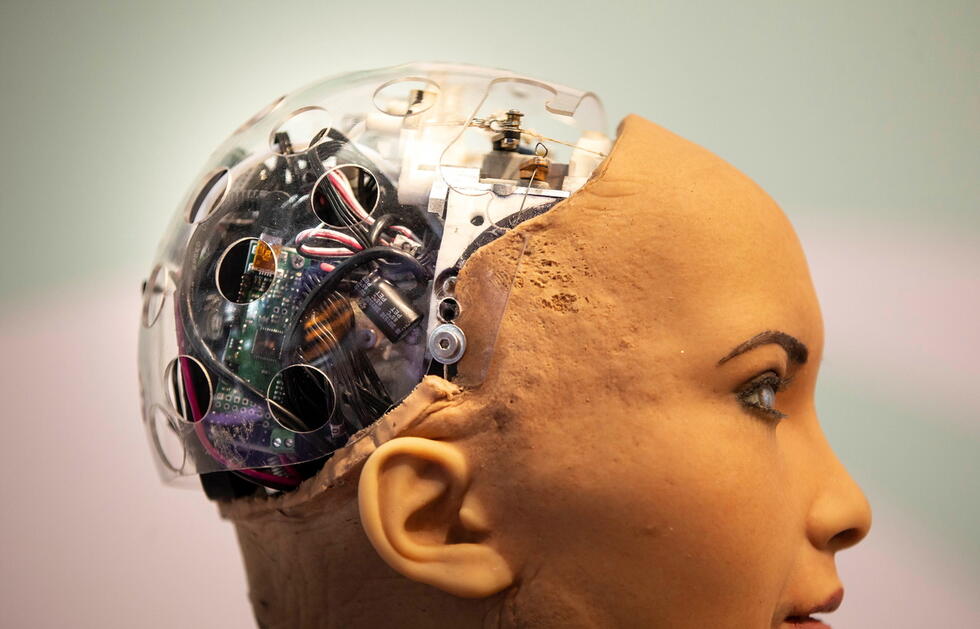
Diagnostics: A new era begins
Artificial intelligence could revolutionize medical diagnostics – for example the algorithm developed by the pathologist Viktor Kölzer. But this revolution requires data. And data requires protection.

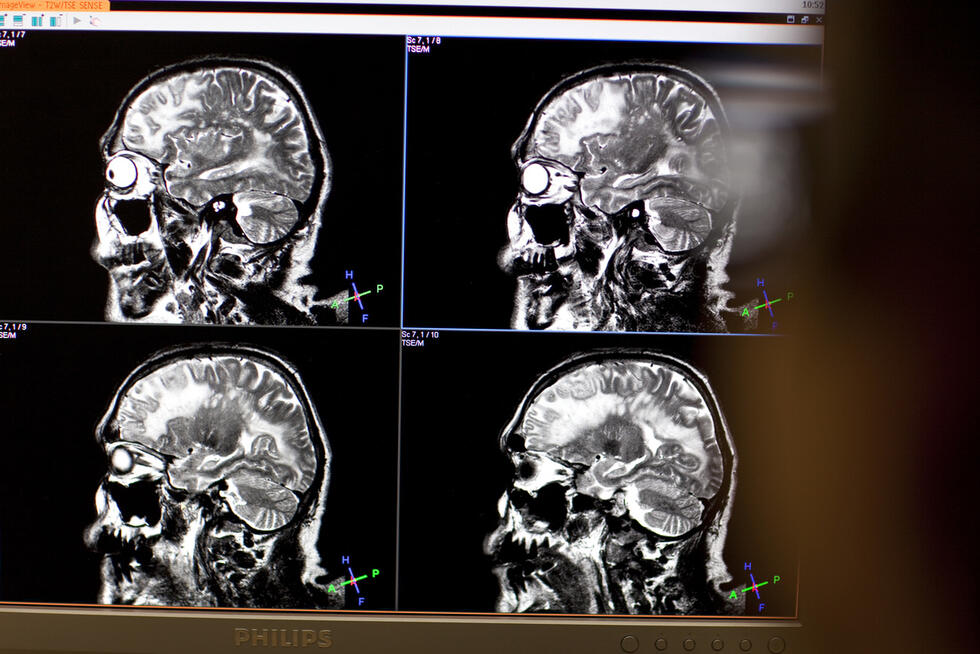
They examine hundreds of x-rays, scarcely ever overlooking a suspicious detail. Their decisions are consistent. And they identify correlations even in vast volumes of complex medical data: Artificially intelligent diagnostics systems have the potential to revolutionize the identification of diseases. Simply because they are capable of doing things that neither humans nor other technologies have been able to do until now. The consequences: more highly targeted treatments and a reduction of unnecessary costs and patient risks.
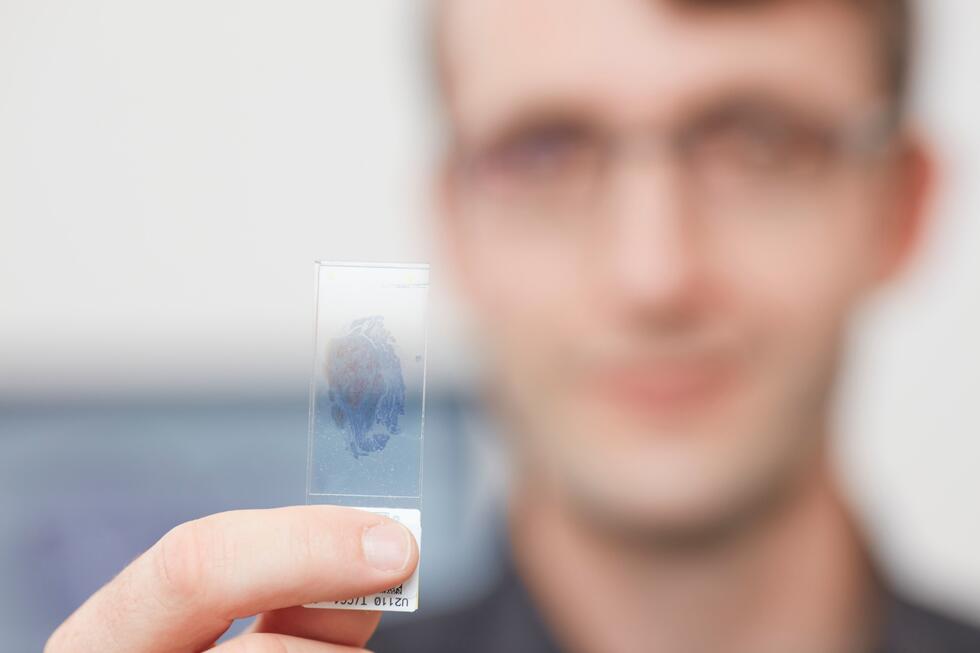
This is precisely the potential offered by the system that is being developed by the international research team led by Viktor Kölzer, Professor of Computer-Aided Image Analysis in Pathology at the Zurich University Hospital. The system’s artificial intelligence enables a new type of classification of colon tumors – and it usually hits the mark. To achieve this, the algorithm combines data from two areas: The first is tissue sections. For more than a century, pathologists have been examining these under the microscope in order to accurately classify diseases. The other area – RNA sequencing – by contrast, is a brand new method. It provides a fingerprint, so to speak, of the tumor’s gene activity and can thus reveal valuable additional insights for the prognosis and thus also for treatment. The new algorithm combines both methods and thus analyzes both image and gene expression data. In this way, the system generates information that has never been available before.
Three phases
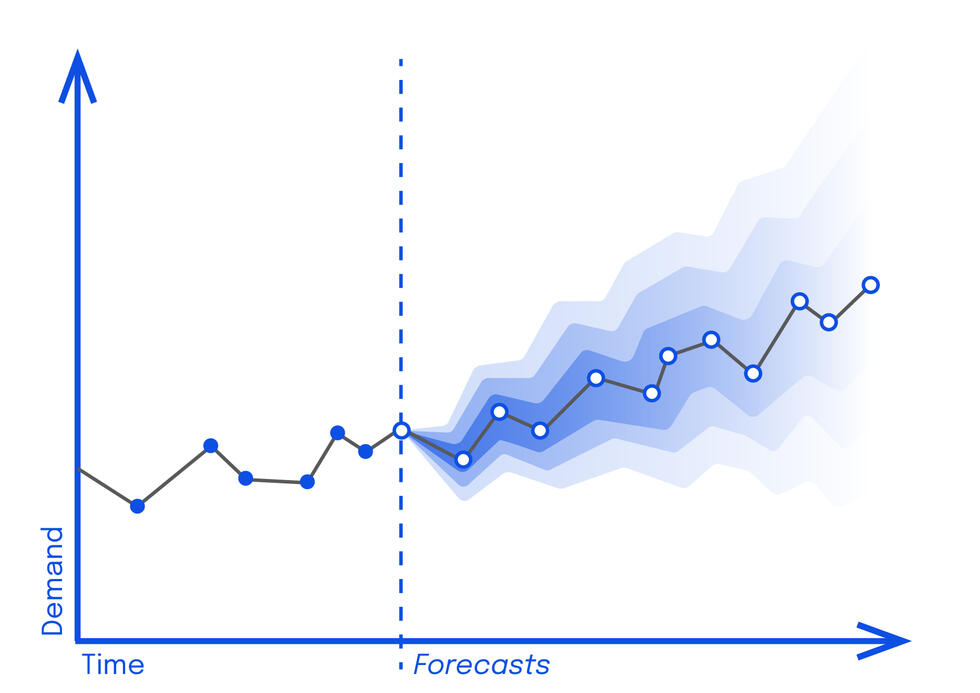
Artificial intelligence and medicine are still a young team. The pathologist Viktor Kölzer expects that AI will find its way into diagnostics in phases:
Phase 1
Artificial intelligence systems support medical specialists by performing repetitive tasks, such as the examination of x-rays. “AI never gets tired and performs consistently compared to humans.” This also boosts cost efficiency.
Phase 2
In this phase, AI combines different types of data, recognizes new patterns in large, complex datasets, and makes predictions on this basis, Viktor Kölzer explains.
Phase 3
“Here we are talking about what is known as strong AI, which is at least equal to human intelligence and acts independently. However, such systems do not exist yet. And it is possible that they will only be used to a limited extent in medical applications.”
How reliable are the systems?

As strong as the potential of AI in diagnostics is, the question remains as to what extent such systems can be trusted. In particular when they are involved in the diagnosis of potentially lethal diseases. The emphasis here is on the word “involved”. “In current medical practice, AI never makes decisions on its own and performs best in the hands of human specialists,” Viktor Kölzer emphasizes. “And these specialists should view the AI’s findings as pointers, not facts.” When it comes to the medical ethicist Markus Christen, the chief physician and researcher is preaching to the converted: “Naturally, the question of trust is particularly important in the medical field,” says the Managing Director of the University of Zurich’s Digital Society Initiative (see box). “However, this applies to all tools, not just to the intelligent ones.”
Nevertheless, for the latter, the possibility of increasing the reliability is growing: by means of “Explainable AI” (XAI). This young branch of AI research aims to make the decisions of algorithms more comprehensible to humans. Viktor Kölzer and his team are also working with XAI. Another way to verify the reliability of algorithms is to validate them using as many different datasets as possible. Viktor Kölzer: “The more data that is available for this purpose worldwide, the better. Without sufficient – digitally recorded – data and the opportunity for international exchange, we will not be able to make further progress in the field of AI.”
Critically scrutinizing digitalization
The University of Zurich’s Digital Society Initiative is an interdisciplinary center that focuses on digital change in the various fields of research and teaching – for instance in medicine. The aim is to critically reflect on the process of digitalization and to shape it in a future-oriented manner. More information: www.dsi.uzh.ch
Find out more about the new algorithm developed by Viktor Kölzer and his research team:
http://gut.bmj.com/cgi/content/full/gutjnl-2019-319866
Major challenge: data privacy
So let’s now address the pivotal challenge relating to AI: data privacy. “The existing Swiss Data Protection Act is definitely not yet optimally tailored to the new applications,” says Markus Christen. And he immediately follows up with a possible approach towards solving this issue: “The data from one sphere of life should not be allowed to leave its confines.” As a rule, people who have agreed to the use of their data in pathology would generally not object to it also being used in oncology. “However, they would rightly object if, all of a sudden, their data is also used by insurance companies or banks,” Markus Christen explains. “If instead of the minor boundaries – between individual fields of research or projects – the major boundaries were defended, medicine would suddenly gain access to much more data.”
An even more typical ethical problem related to AI: How representative is the data that was used to train the algorithm? In principle, according to both Markus Christen and Viktor Kölzer, algorithms have the potential to make decisions that are much more nondiscriminatory than, for example, a small team of physicians. This, however, only applies if the data used for training also adequately reflects, for example, all the relevant patient groups: “The more unbiased the data, the more unbiased the decisions made by the intelligent system.”
Huge step in developing countries
This also means that an AI system cannot simply be transferred to another part of the world. For example, the intelligent procedure from Oxford University, which reputedly outperforms British cardiologists in the diagnosis of heart disease, will not necessarily achieve the same results in Malawi. On the one hand because of the training data: For the system to perform equally as well, it would have to be trained using local patient data. But other technical requirements also play a role: simply using a different scanner can irritate the AI. “The AI can learn such differences and take them into account,” Markus Christen explains. “If it fails to do so, its results will be skewed.”
Especially in diagnostics, algorithms can provide people with access to methods that might otherwise be completely missing
When all these factors are taken into account, AI systems mean one thing above all for developing countries: a giant leap forward. “In certain regions of Africa, for example, there are only very few specialists for each medical field,” Viktor Kölzer emphasizes. “Especially in diagnostics, algorithms can provide people with access to methods that might otherwise be completely missing.” Such methods can be made available to hospitals or medical practices – or, thanks to the widespread use of smartphones, directly to the patients. For example in the form of apps that analyze moles or measure blood sugar and heart rate.
Inexpensive access to modern cancer diagnostics
At least in our part of the world, the colon cancer algorithm developed by Viktor Kölzer’s team – which is currently being tested to determine whether it can be generalized – could soon constitute a major step forward. “If the system proves successful, we will be able to make it available at very low cost – for five to ten Swiss francs per patient,” Viktor Kölzer explains. In comparison: Conventional RNA sequencing – which, albeit, also provides important additional information for cancer diagnostics – costs around 1000 Swiss francs per patient.
Early detection and prevention: wearable devices
Direct access to simple medical applications constitutes a massive added value, not only in developing countries. “Wearables open up completely new possibilities for everyone. These assistive devices comprise a wide variety of intelligent mobile objects – watches, clothes, adhesive plasters. A study by the Scripps Research Institute in California, for example, has shown that plasters that independently measure the ECG of high-risk heart patients are three times more effective than regular hospital check-ups. The pathologist Viktor Kölzer explains: “Good healthcare devices can significantly improve the early detection and prevention of diseases. At the same time, patients are given the opportunity to collect their own health-related data, to evaluate it using AI, and to make use of it themselves.” However, this is a development that should not be taken uncritically: “In authoritarian states, such devices can be abused as data sources for social control,” the medical ethicist Markus Christen says. “Thus a social debate on the ethical and legal framework of such systems is essential.”
Written by:
Photos: sda-keystone