Robots revolutionize neurosurgery
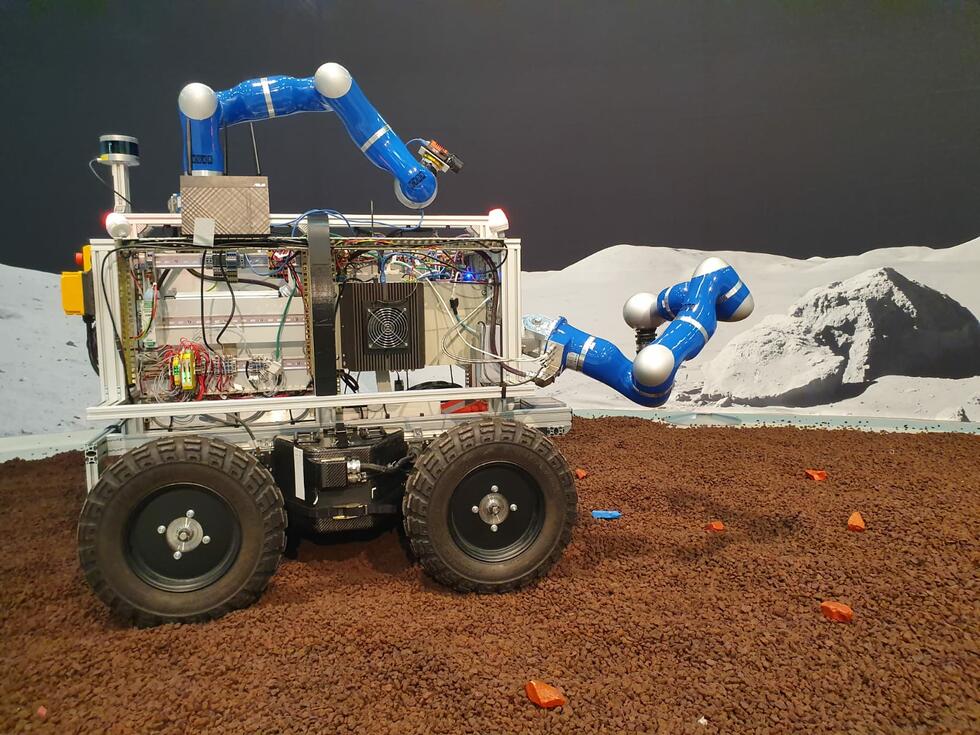
Robots were intended to advance surgery to the next level. Instead, they fell into disrepute as a result of medical errors and high costs. To date, brain surgery is the field where the technology can best play to its strengths. The robotic assistants increase the precision and efficiency of delicate procedures.
Expectations for the Da Vinci surgical robot were high: reduced blood loss, less pain, and shorter recovery times. But the market launch in 2000 was ill-fated. In the United States, several surgical incidents occurred, some of these with fatal consequences.
Nevertheless, the technology has established itself. Today, Da Vinci is being used by numerous hospitals to treat prostate and uterine cancer. However, the benefits of the surgical robot remain a subject of controversy. The operations are significantly more expensive than manual procedures and take approximately the same time.
Also from a medical viewpoint, the high investments only pay off to a limited extent. The Swiss Medical Board sees no significant advantages compared to conventional surgery. The same conclusion was reached by studies conducted in the United States and Australia.
Twice as fast as by hand
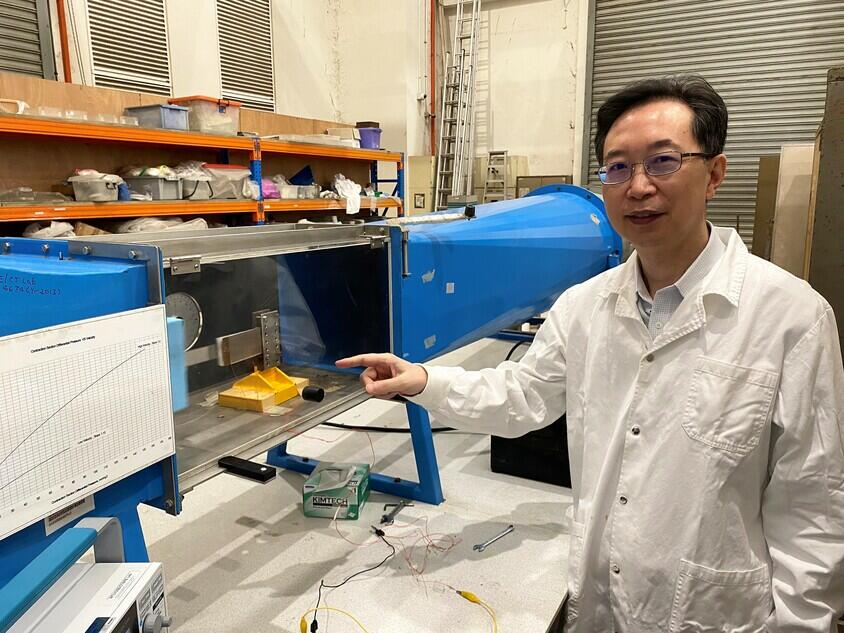
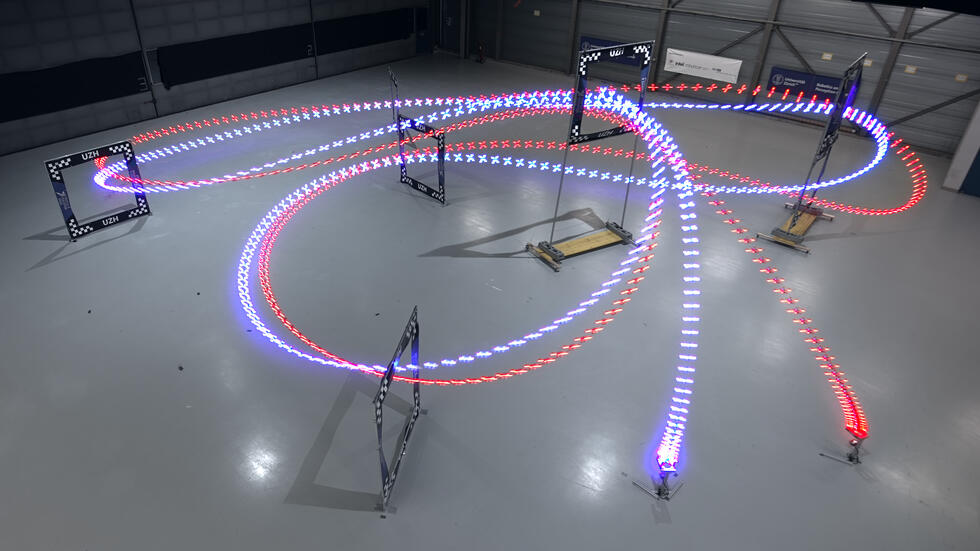
The potential of robotics appears to be greater in the field of neurosurgery. Here, the most promising technology is called Neuromate. “The robot allows us to reach our goal much more quickly,” says Niklaus Krayenbühl from the University Children’s Hospital Zurich. Over the past two years, the neurosurgeon has performed some 35 robot-assisted operations on children between the ages of two and 14. On average, the procedures took about half as long as they would have if performed using conventional methods.
The surgeon appreciates the robot’s precision, because neurosurgery requires extreme accuracy: “The margin of tolerance is usually below one millimeter,” Niklaus Krayenbühl emphasizes. Surgery on infants is particularly critical because their organs are still small and very fragile.
The robot performs more precisely than the best surgeon’s hands – which does not mean that these are not still needed: “The robot merely assists. As yet, fully automated surgery is not feasible.”
Surgery without detours
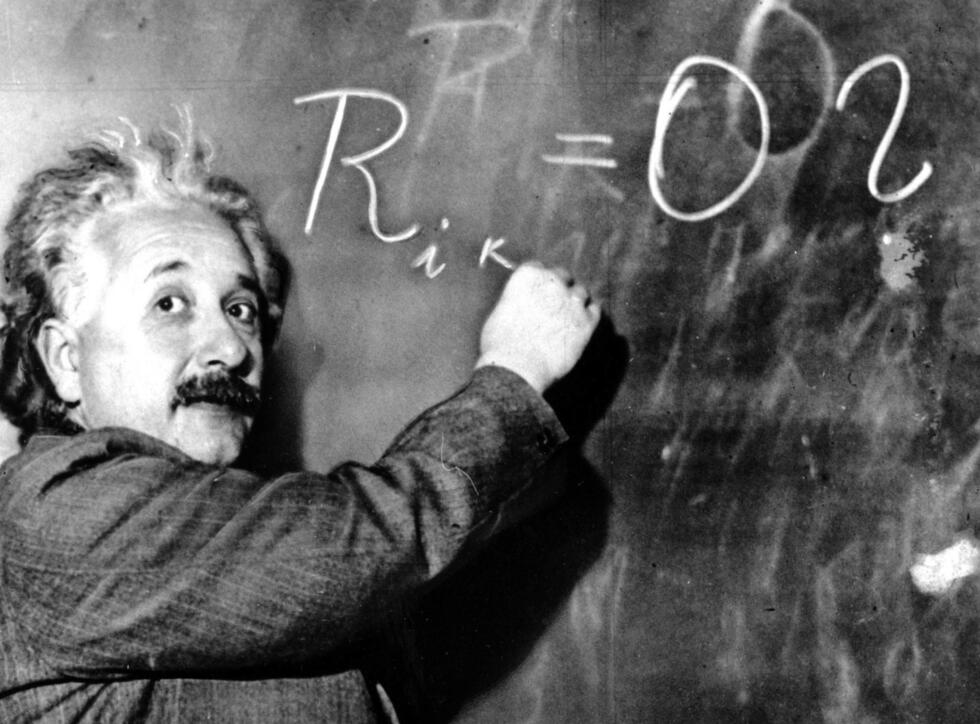
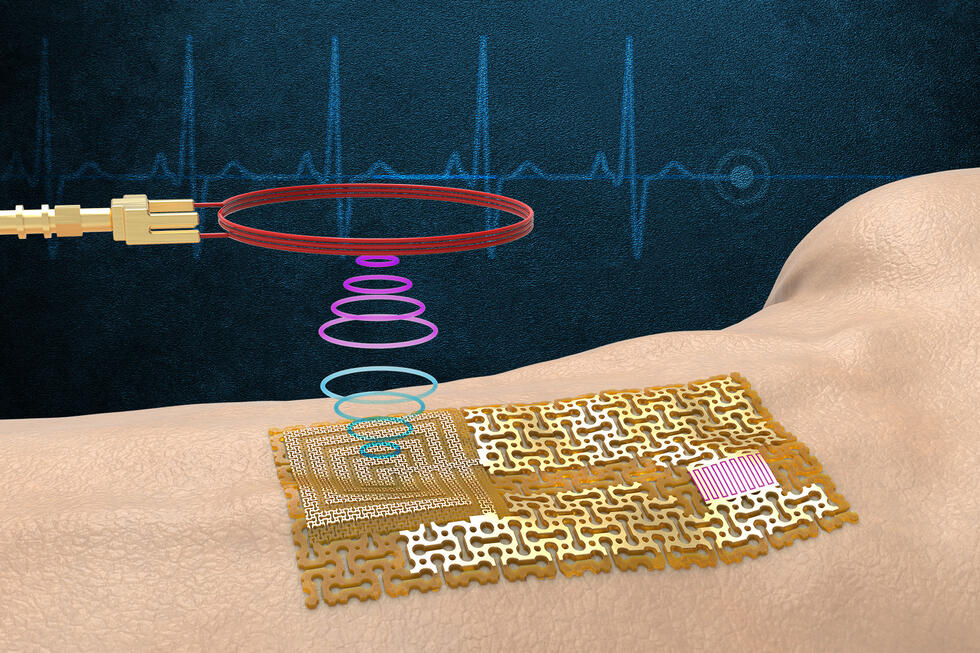
The machine assistant simplifies the complex procedure of stereotaxy, which has facilitated high-precision brain surgery since the 1940s. Stereotactic surgery involves immobilizing the patient’s head in a rigid frame. A three-dimensional coordinate system allows brain areas to be targeted with pinpoint accuracy using stereotactic systems. The Neuromate handles the complex navigational process and the alignment with the X-ray, CT, and MRI images.
“This means that we can work much more directly,” Niklaus Krayenbühl explains. “We can target brain areas in a 3D model and perform all the tasks with the robot’s assistance – from drilling to the positioning of needles or electrodes. We used to have to first transfer the coordinates from the screen to the frame and then manually manipulate the instruments. And since the robot is much more rigid than the conventional ring system, it also enables a higher level of precision.”
Sights set on brain tumors and epilepsy
The surgical robot offers support in the fight against a wide variety of brain diseases such as Parkinson’s or Tourette’s syndrome. The University Children’s Hospital Zurich uses it primarily for the diagnosis of tumors and epilepsy. Most of the applications involve extracting tissue samples from deep-seated or particularly delicate areas of the brain. The system is also capable of implanting electrodes to diagnose therapy-resistant epilepsy. It can also be used to insert catheters that allow the injection of drugs or laser probes to destroy pathological brain tissue.
“We were already able to perform all of these procedures manually, but it was very difficult work,” Niklaus Krayenbühl says. Implanting electrodes during a stereoelectroencephalography (SEEG) procedure used to take five hours. With the robot, it now takes only two.
We can now reach certain areas in the cerebellum and brainstem more easily.
The robot also opens up new capabilities: “We can now reach certain areas in the cerebellum and brainstem more easily. Previously, targeting them could be difficult because the angle of the stereotactic systems was limited.”
New player in a monopolistic market
In 2019, the University Children’s Hospital Zurich became the first Swiss hospital to deploy the Neuromate. Meanwhile, the device is also in use at the University Hospitals of Geneva and Zurich. Robots are already widely used in Swiss operating theaters: Switzerland boasts the highest density of surgical robots in the world. Currently, more than 30 are in use in hospitals throughout the country. Per capita, that is almost three times as many as in Germany.
All the surgical robots in Switzerland – with the exception of the three Neuromates – are Da Vinci robots. Its US manufacturer Intuitive Surgicals holds a de facto monopoly in the market for surgical robots. The system’s reputation as a cost creator is not without reason: The device costs almost two million Swiss francs. On top of that, the maintenance and tooling costs are also high.

At around 400,000 Swiss francs, the Neuromate is considerably cheaper. The University Children’s Hospital Zurich is confident that the time saved during surgery makes up for the additional maintenance costs. The higher precision could also help reduce complications and thus save additional costs.
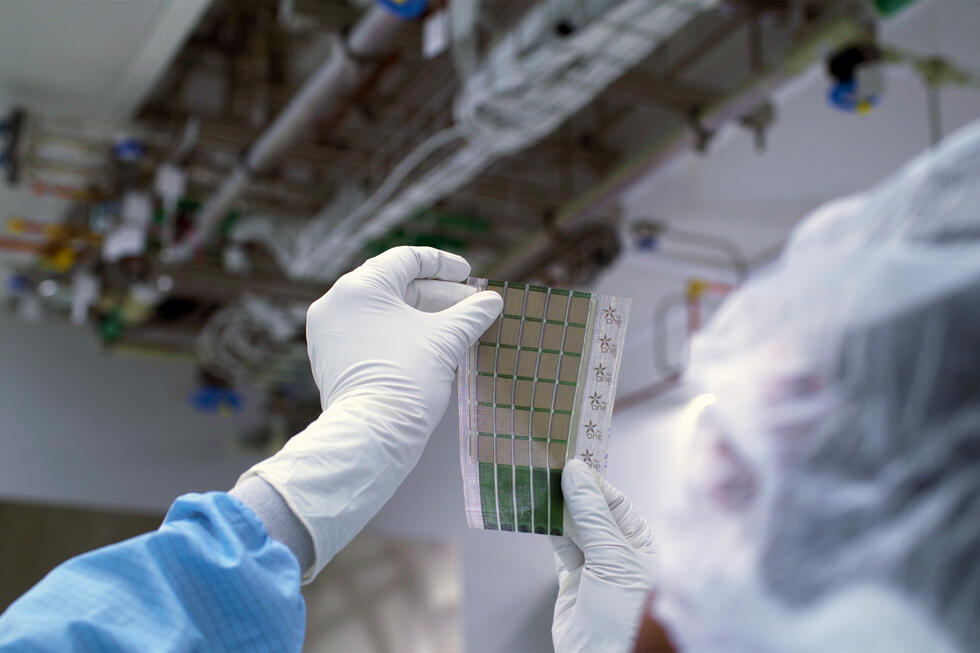
Unlike the market leader from California, medtech is not the core business of Renishaw, the supplier of Neuromate. The British company originally specialized in measurement technology for industry, and its product range now also includes systems for industrial 3D metal printing. In recent years, the manufacturer has increasingly shifted its know-how to medical technology: The company acquired the technology for the Neuromate by means of a takeover in 2008. In the meantime, Renishaw has also started offering solutions for the 3D printing of prostheses.
Artificial intelligence sees more
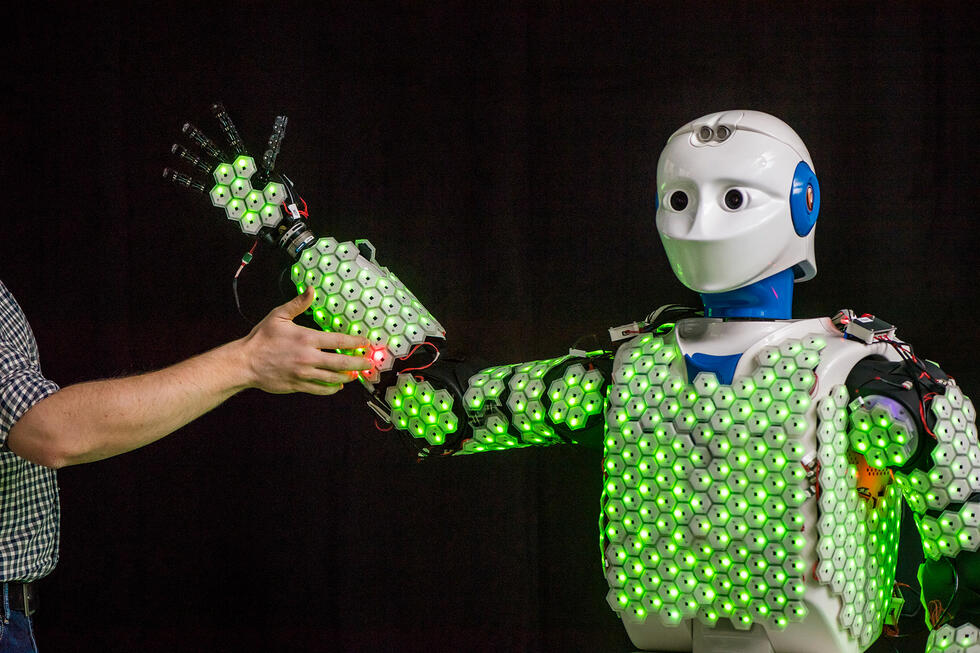
In addition to neurosurgery and urology, robots are already being used for individual applications in the field of prosthetics, for example to implant artificial hip joints. As different as the areas of application are, all surgical robots have one thing in common: They minimize the tissue damage caused by surgery.
They thus support the trend toward minimally invasive surgery that began in the 1990s. Microsurgery, which – like brain surgery – involves the use of highly augmentative visual aids, is also likely to benefit from this trend. “Robots are helping to make microsurgery even more precise and patient-friendly,” Niklaus Krayenbühl says.
In the diagnosis of epilepsy, artificial intelligence could potentially be of great service to us.
In addition to robotics, there are other new technologies that are key to the further development of surgery: “Molecular diagnostics and personalized medicine will result in progress in the coming years,” says Krayenbühl with conviction. The neurosurgeon also believes in the potential of artificial intelligence: “Image analysis is one of the main strengths of AI. In the diagnosis of epilepsy, the technology could potentially be of great service to us.”





About Niklaus Krayenbühl, neurosurgeon at the University Children’s Hospital Zurich
In early 2021, Professor Niklaus Krayenbühl, MD, was appointed Switzerland’s first chief pediatric neurosurgeon. The 51-year-old joined the University Children’s Hospital Zurich in 2017. His main focus is on the treatment of pediatric brain tumors and epilepsy surgery. The University Children’s Hospital Zurich is a pioneer in this field. Its EEG department, which specializes in epilepsy diagnostics for children, was founded as early as 1953.
Written by:
Illustration: Liebana Goñi